News
|
Shape Divider - Style fan_opacity
|
The Value of Value-Based HealthcareIs It Time for Your Practice to
|
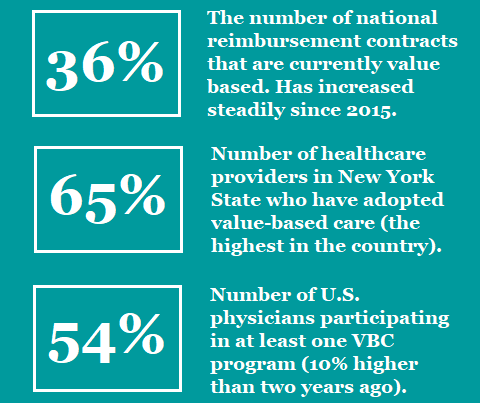
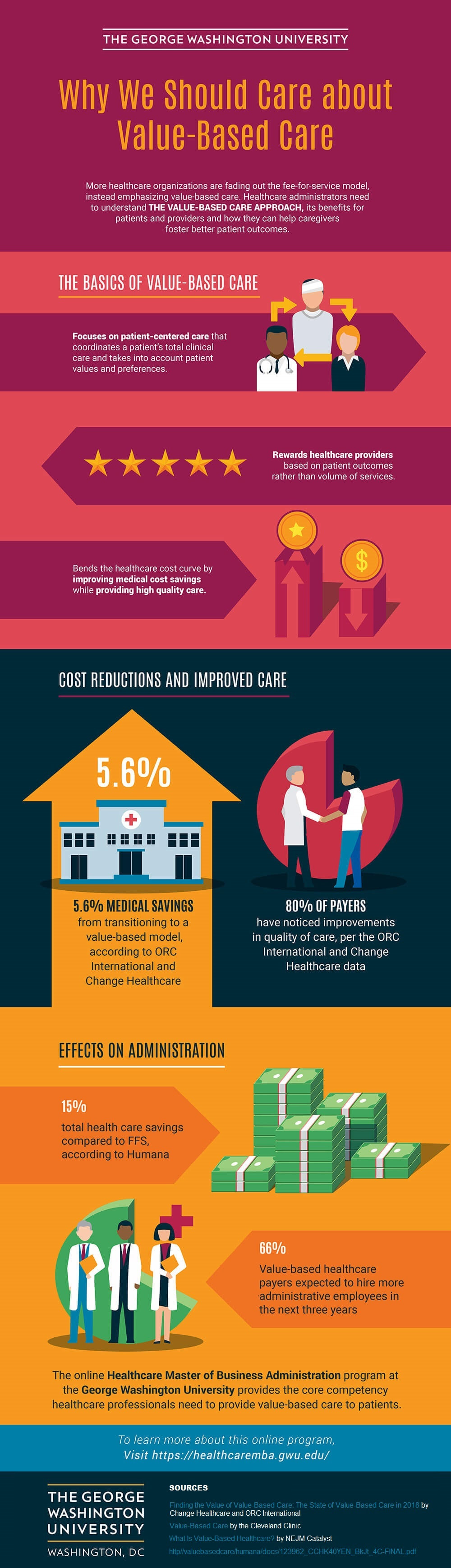
Unlike the FFS model, VBC is data-driven. Providers must track and report specific metrics (e.g., hospital readmissions and population health) in order to determine health outcomes. Current government regulations strongly favor value-based care over traditional reimbursement models. VBC Payment Models
There are four main types of value-based payment models available for providers.
Accountable Care Organizations (ACO) An ACO is a network of healthcare providers of varying specialties who voluntarily work together to offer coordinated care to their patients. Originally designed for Medicare beneficiaries, ACOs have now expanded to include patients covered by private insurers. Their purpose is to prevent redundant and unnecessary services while also reducing medical errors. Whenever the ACO is able to provide quality care and services at reduced costs for patients, all providers within the network share in the savings. Of course, they also share in the losses if care quality is not adequate, so there is some financial risk to joining an ACO. Providers who do not meet the standard for value-based care may have to repay Medicare or the private insurer. |
Bundled payments (or episode-based payments) allow patients to pay a single price for an entire episode of care, even if they were treated by multiple providers. Providers are reimbursed collectively for the pre-determined costs to treat a specific condition that may include several practitioners, care settings, and procedures. Payment is based on treatment outcome.
For instance, if a patient undergoes surgery, a single payment to the hospital, surgeon, and anesthesiologist would be bundled together based on historical prices instead of paying each provider separately.
As with ACOs, providers who offer bundled payments assume certain risks. Any treatment costs above the target price for an episode of care (such as those arising from complications or hospital readmissions) must be covered by the healthcare provider. By the same token, whenever costs are kept below the bundled price, providers share the savings.
A PCMH is not simply a place; it’s a model for primary care. PCMHs are similar to ACOs in that they involve a group of providers working together to provide all-inclusive care services to their patients. PCMHs focus on five main attributes:
The PCMH model is particularly effective in improving care coordination with patients who suffer from complex chronic disease. Practice facilities may become PCMH certified through several different accreditation programs.
Capitation
Capitation is another VBC payment model. With this model, providers receive in advance a fixed fee per patient which is based on several factors (such as demographic data, range of services provided, and number of patients involved). Like the other VBC models, the goal of capitation is to reduce both excessive care services and overcharging, by delivering services through a primary care provider and inpatient procedures.
This model focuses on prevention and treatment, outpatient lab tests, immunizations and other prescribed injections, vision and hearing screening, and health education.
Value-Based Care Benefits
Better Healthcare for Less Money
With VBC, providers are far less likely to recommend services their patients may not need or treatments that may not work. When practitioners focus on providing personalized solutions to their patients’ underlying health issues, better outcomes are achieved.
|
Improved Patient Satisfaction
Patient satisfaction is key in value-based care. By offering more personalized treatment solutions, practitioners can ensure a more positive patient experience. And satisfied patients are more likely to return and recommend your practice to others. Improved Care Coordination In VBC, incentives and improved technologies facilitate coordination of care with multiple providers. This collaboration creates better patient outcomes because all of their care providers are working together to improve overall health. A Healthier Society Patients with chronic conditions are more likely to address their medical issues early, and take control of their disease, if healthcare costs are affordable and providers personalize their services. VBC helps create a more financially stable population that seeks treatment for long-term illnesses through the best care methods available. The Future of Healthcare
Value-based care models are becoming increasingly popular, as the Department of Health and Human Services continues to attract providers to these alternative payment models by offering incentives. (For instance, practitioners who successfully transition to VBC could increase their Medicare Part B base payment rate by as much as nine percent, with the possibility of additional lump sum payments.)
In our current environment of ever-increasing healthcare costs, VBC has become a critical part of the prudent provider’s strategy to generate revenue and contain costs. Those providers who begin now to shift their focus from care and treatment to prevention and health maintenance are positioning themselves for the future. |
One of the primary challenges for practitioners who wish to adopt value-based care is effectively tracking the required metrics. In order to calculate cost of healthcare, providers must track a bevy of data, such as staffing, clinical information, population health data, patient acuity, etc. Most hardware, software, and internal processes currently being used by providers are designed to accommodate FFS care models. Choosing the right VBC technology partner will be important. For a comparison of value-based care services and vendors, click here. In addition, an organization’s internal culture may be resistant to adopting value-based payment models, having built its entire approach around FFS healthcare. Providers must undergo a paradigm shift from “volume and claims” to “value and health outcomes.” This will require training and adjustment time in order to facilitate a smooth transition. |
Featured Image: Adobe, License Granted
RevCycle Intelligence
Health IT Analytics
Software Advice
CapMinds
Agency for Healthcare Research and Quality
Contact Information
Address2150 Lelaray Street
Colorado Springs, CO 80909 P.O. Box 140 Colorado Springs, CO 80901 |
ContactPhone: (800) 266-3809 / (719) 634-3760
Email: [email protected] Business Hours: Monday – Friday, 8am – 5pm Closed Sat/Sun |
Other Information |